Behandling av nedsunken livmor
Behandlingen av nedsunken livmor avhenger av hvor svakt støttevevet rundt livmoren er blitt. Ved milde og beskjedne plager vil man ikke anbefale behandling. I tilfeller der behandling er nødvendig, kan dette være bekkenøvelser, medisiner, pessar eller operasjon.

Sist oppdatert:
30. juni 2025
Innhold i artikkelen
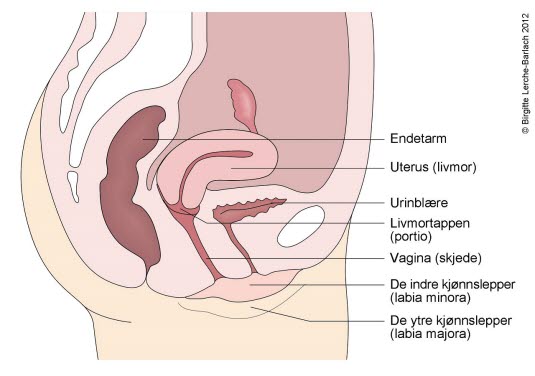
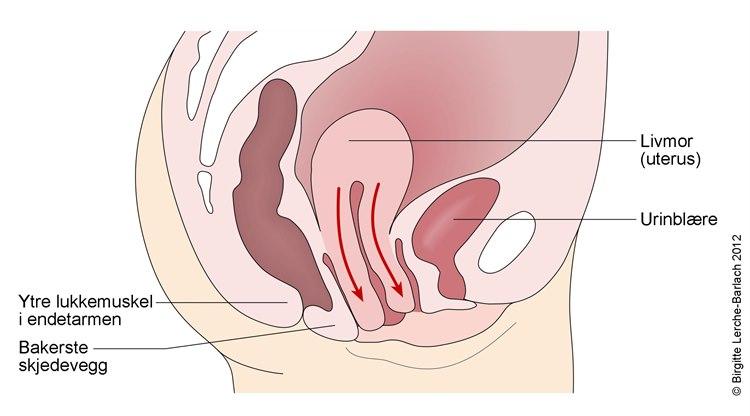
Nedsunken livmor, livmorfremfall eller livmorprolaps, oppstår når muskulaturen i bekkenbunnen strekkes og svekkes slik at støtten til livmoren minsker. Livmoren vil da sige ned og i uttalte tilfeller kunne stikke ut av skjeden.
Hvis du har et beskjedent eller mildt livmorfremfall, enten uten symptomer eller med symptomer som ikke plager deg, vil du sannsynligvis ikke behøve behandling. Men hvis bekkengulvet fortsetter å svekkes, så vil fremfallet kunne bli tiltakende plagsomt. Da kan det bli aktuelt med behandling.
I mange tilfeller kan du forhindre forverrelse ved å unngå overvekt og ved å unngå tunge tak og løft, samt drive med bekkenøvelser.
Unge kvinner som har fått nedsunken livmor etter en fødsel, vil man vanligvis ikke anbefale operasjon før det er gått minst ett år etter fødselen. De fleste av disse tilfellene går nemlig tilbake av seg selv.
Bekkenøvelser
Du kan styrke bekkenmusklene ved å drive med øvelser hjemme. Det gjør du ved å stramme bekkenmusklene som om du prøver å stanse urinstrømmen når du tisser. Sett av ti minutter flere ganger daglig til slike knipøvelser. Øvelsen styrker bekkenbunnen og gir noe støtte. Slike øvelser kan reduserer plagene i de tilfellene der prolaps (nedsunken livmor) foreligger.
Medisiner
Østrogenkrem som sprøytes inn i skjeden, eller som stikkpiller, hjelper til med å gjenskape styrke og vitalitet i vevet i skjeden. Slik behandling tilrås til alle kvinner med nedsunken livmor etter overgangsalderen. Det kan i milde tilfeller være eneste nødvendige behandling.
Kirurgi
Avhengig av alderen og graviditetsønske, kan kirurgi enten brukes til å styrke opphengningen av livmoren, eller man kan fjerne livmoren (hysterektomi). Før inngrepet anbefales forbehandling med østrogenkrem i skjeden i minst 2 uker.
I forbindelse med inngrepet kan kirurgen stramme opp skjedeveggene, urinblæren, endetarmen og rette ut urinrøret. Etter inngrepet er det ikke uvanlig med mindre komplikasjoner i form av lette blødninger, infeksjon, blærekatarr, blæretømningsproblemer og urinlekkasje. Dette er imidlertid som regel forbigående plager eller besvær som er lett å behandle.
Det er viktig å drive med bekkenøvelser etter et slikt inngrep fordi uten øvelser kan opptil 25 prosent få problemer med urinlekkasje. Kvinner etter overgangsalderen blir vanligvis også anbefalt lokalbehandling med østrogenkrem.
Annen behandling
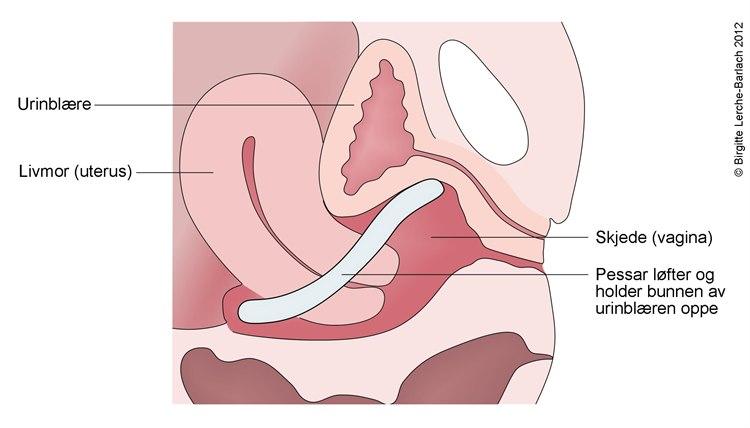 Pessar
PessarDersom operasjon ikke er ønskelig eller vurderes som en stor belastning, kan behandling med pessar være et alternativ. Pessaret plasseres i skjeden og bidrar til å forhindre at livmoren synker ned. Det kan brukes midlertidig eller som en varig løsning. Pessar finnes i ulike størrelser og tilpasses individuelt. Ved store prolaps vil ikke et pessar hjelpe. Et dårlig tilpasset pessar kan dessuten gi ubehag i fra skjeden i form av gnagsår og plagsom utflod. I slike tilfeller med ubehag er det ofte nok å fjerne pessaret for et par uker og så sette det inn igjen. Hos enkelte kan det hjelpe å få penslet såret som har dannet seg på livmortappen. Intensivert østrogenbehandling vil også bidra til rask bedring. Et pessar bør rengjøres hver 3. til 6. måned, og dette gjøres vanligvis hos lege.
Oppfølging
Oppfølgingen avhenger av hvordan tilstanden behandles. Ved gjennomført operasjon er det behov for kontroller hos kirurg. Ved bruk av pessar i skjeden, bør dette rengjøres og kontrolleres jevnlig hos lege, for eksempel én gang i halvåret. Ved pågående bekkenbunnstrening vil lege kunne følge opp og vurdere effekten av treningen
Forebygging
- Gå ned i vekt om du er overvektig.
- Unngå forstoppelse ved å holde et grovt kosthold og ha gode toalettvaner.
- Unngå tunge tak og løft.
Prognose
Pessar kan være effektivt både forbigående og permanent hvis det kontrolleres og rengjøres regelmessig. Operasjon som "strammer opp" de innvendige organene, gir svært ofte gode resultater, men det forekommer tilbakefall i opptil 20 prosent av tilfellene. Færre enn fem prosent behøver ny operasjon. I en spørreundersøkelse av opererte pasienter anga cirka 95 prosent at de var fornøyde med resultatet.
Fjerning av livmoren løser problemet en gang for alle.
Dette dokumentet er basert på det profesjonelle dokumentet Genitalprolaps . Referanselisten for dette dokumentet vises nedenfor
- Oversand S, Eidet M, Rimstad K, McFadzean I. Descensus urogenitalis (2021). Veileder i generell gynekologi. Oslo: NGF; sist oppdatert 19.01.10125. Siden besøkt 27.06.2025 metodebok.no
- Iglesia CB, Smithling KR. Pelvic Organ Prolapse. Am Fam Physician. 2017 Aug 1;96(3):179-185. PMID: 28762694. PubMed
- Collins S, Lewicky-Gaupp C. Pelvic Organ Prolapse. Gastroenterol Clin North Am. 2022 Mar;51(1):177-193. PMID: 35135661 PubMed
- Nygaard I, Barber MD, Burgio KL et al. Prevalence of symptomatic pelvic floor disorders in US women. JAMA 2008; 300: 1311-6. Journal of the American Medical Association
- Schaffer JI, Wai CY, Boreham MK. Etiology of pelvic organ prolapse. Clin Obstet Gynecol 2005; 48: 639-47. PubMed
- Barber MD, Maher C. Epidemiology and outcome assessment of pelvic organ prolapse. Int Urogynecol J. 2013;24(11):1783-90. PubMed
- Haylen BT, Maher CF, Barber MD, et al. An International Urogynecological Association (IUGA) / International Continence Society (ICS) Joint Report on the Terminology for Female Pelvic Organ Prolapse (POP). Neurourol Urodyn 2016. PMID: 26749391. PubMed
- Schulten SFM, Claas-Quax MJ, Weemhoff M, et al. Risk factors for primary pelvic organ prolapse and prolapse recurrence: an updated systematic review and meta-analysis. Am J Obstet Gynecol. 2022 Aug;227(2):192-208. PMID: 35500611 PubMed
- Deprest JA, Cartwright R, Dietz HP, et al. International Urogynecological Consultation (IUC): pathophysiology of pelvic organ prolapse (POP). Int Urogynecol J. 2022 Jul;33(7):1699-1710. PMID: 35267063 PubMed
- Barber MD. Pelvic organ prolapse. BMJ. 2016 Jul 20;354:i3853. PMID: 27439423 PubMed
- Svenningsen R, Borstad E, Spydslaug AE, Sandvik L, Staff AC. Occult incontinence as predictor for postoperative stress urinary incontinence following pelvic organ prolapse surgery. Int Urogynecol J. 2012;23(7):843-9 PubMed
- Hagen S, Stark D. Conservative prevention and management of pelvic organ prolapse in women. Cochrane Database of Systematic Reviews 2011, Issue 12. Art. No.: CD003882. PMID: 22161382 PubMed
- Sansone S, Sze C, Eidelberg A, et al. Role of Pessaries in the Treatment of Pelvic Organ Prolapse: A Systematic Review and Meta-analysis. Obstet Gynecol. 2022 Oct 1;140(4):613-622. PMID: 36075076 PubMed
- Rahn DD, Carberry C, Sanses TV, et al. Vaginal estrogen for genitourinary syndrome of menopause: a systematic review. Obstet Gynecol. 2014;124(6):1147-1156. PubMed
- Hagen S, Glazener C, McClurg D et al. Pelvic floor muscle training for secondary prevention of pelvic organ prolapse (PREVPROL): a multicentre randomised controlled trial. Lancet 2017; 389(10067): 393-402. pmid:28010994 PubMed
- Hagen S, Stark D, Glazener C, et al. Individualised pelvic floor muscle training in women with pelvic organ prolapse (POPPY): a multicentre randomised controlled trial. Lancet 2013 Nov 27.
- Wiegersma M, Panman CM, Kollen BJ, et al. Effect of pelvic floor muscle training compared with watchful waiting in older women with symptomatic mild pelvic organ prolapse: randomised controlled trial in primary care. BMJ. 2014 Dec 22;349:g7378. PubMed
- Panman C, Wiegersma M, Kollen BJ, et al. Two-year effects and cost-effectiveness of pelvic floor muscle training in mild pelvic organ prolapse: a randomised controlled trial in primary care. BJOG. 2016- PMID: 26996291 PubMed
- Braekken IH, Majida M, Engh ME, Bo K. Can pelvic floor muscle training reverse pelvic organ prolapse and reduce prolapse symptoms? An assessor-blinded, randomized, controlled trial. Am J Obstet Gynecol. 2010 Aug;203(2):170.e1-7. PMID: 20435294 PubMed
- Rudnicki M, Laurikainen E, Pogosean R, et al. Anterior colporrhaphy compared with collagen-coated transvaginal mesh for anterior vaginal wall prolapse: a randomised controlled trial. BJOG 2013. pmid:24118844 PubMed
- Altman D, Väyrynen T, Engh ME, et al. Anterior colporrhaphy versus transvaginal mesh for pelvic-organ prolapse. N Engl J Med 2011; 364: 1826-36. New England Journal of Medicine
- Sokol AI, Iglesia CB, Kudish BI, et al. One-year objective and functional outcomes of a randomized clinical trial of vaginal mesh for prolapse. Am J Obstet Gynecol 2012; 206: 86. PubMed
- Heneghan C, Godlee F. Editorial. Surgical mesh repair and patient safety. BMJ Editorial. BMJ 2018; 363: k4231. doi:10.1136/bmj.k4231 DOI
- Yeung E, Baessler K, Christmann-Schmid C, et al. Transvaginal mesh or grafts or native tissue repair for vaginal prolapse. Cochrane Database Syst Rev. 2024 Mar 13;3(3):CD012079. PMID: 38477494 PubMed
- Bo K, Hilde G, Staer-Jensen J, et al. Postpartum pelvic floor muscle training and pelvic organ prolapse--a randomized trial of primiparous women. Am J Obstet Gynecol. 2015 Jan;212(1):38.e1-7.
- Jelovsek JE, Maher C, Barber MD. Pelvic organ prolapse. Lancet. 2007;369(9566):1027-38. PubMed
- Maher C, Feiner B, Baessler K, Christmann‐Schmid C, Haya N, Marjoribanks J. Transvaginal mesh or grafts compared with native tissue repair for vaginal prolapse. Cochrane Database of Systematic Reviews 2016, Issue 2. Art. No.: CD012079. DOI: 10.1002/14651858.CD012079 DOI
- Oversand SH, Staff AC, Spydslaug AE, Svenningsen R, Borstad E. Long-term follow-up after native tissue repair for pelvic organ prolapse. Int Urogynecol J. 2014;25(1):81-9. PubMed