Kronisk hjertesvikt
Hjertesvikt betegner en tilstand der hjertets pumpefunksjon er svekket i forhold til normalt nivå. Hjertet klarer ikke å pumpe tilstrekkelig med blod rundt i kroppen.

Sist oppdatert:
15. juni 2025
Innhold i artikkelen
Hva er hjertesvikt?
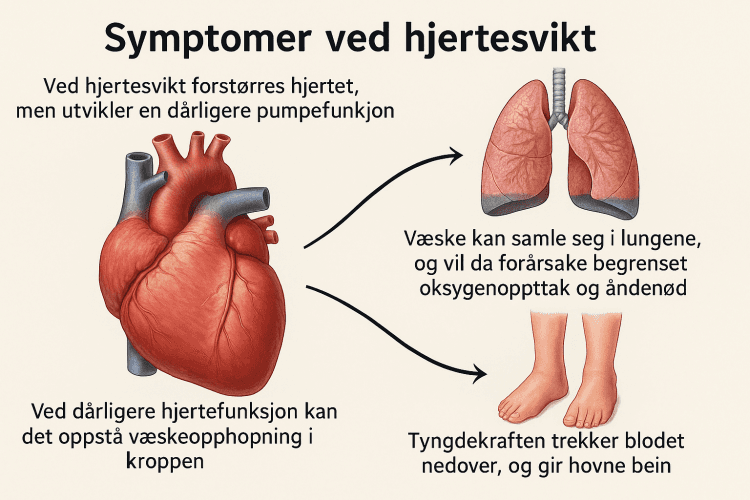
Hjertesvikt er en tilstand der hjertet er svekket slik at evnen til å pumpe blodet rundt i kroppen er redusert sammenlignet med et friskt hjerte. De mest typiske plagene som oppstår, er tung pust og nedsatt fysisk yteevne. Ved lett grad av hjertesvikt merkes dette først ved anstrengelse, mens ved alvorlig hjertesvikt har man tung pust også i hvile. Ved uttalt hjertesvikt vil man kunne merke at pusten blir tyngre når man legger seg ned, og den blir lettere i oppreist stilling. Etter hvert kan det utvikle seg hevelser i beina og ellers i kroppen. Andre symptomer er slapphet, økt trettbarhet, nedsatt matlyst.

Ca 50.000-100.000 personer har hjertesvikt i Norge. Cirka 10 prosent av nordmenn over 70 år har hjertesvikt. Hjertesvikt er årsak til minst 5 prosent av alle akutte sykehusinnleggelser i medisinsk avdeling.
Hjertesvikt, årsaker
Når vi er i bevegelse, øker forbrenningen i kroppen. De aktive kroppsdelene trenger da mer blod for å få nok oksygen og næring. Et friskt hjerte klarer å øke pumpeaktiviteten ved belastning, slik at blodsirkulasjonen blir tilfredsstillende. Et sykt hjerte er ikke i stand til dette, og tilstanden kalles da hjertesvikt.
Forskjellige typer hjertesykdom kan forårsake hjertesvikt. Den vanligste årsaken er et gjennomgått hjerteinfarkt. En del av hjertemuskelen er da død og er erstattet av et stivt arrvev. Dette nedsetter hjertets pumpeevne. Mangeårig høyt blodtrykk vil også kunne slite på hjertet og føre til hjertesvikt. Av samme grunn kan feil på hjerteklaffene (aortastenose, aortainsuffisiens, mitralstenose, mitralinsuffisiens) gi hjertesvikt på grunn av økt belastning og slitasje av hjertemuskelen. Det finnes også en lang rekke tilstander som kan svekke hjertet, for eksempel diabetes, infeksjoner, høyt alkoholforbruk.
Animasjon av hjertesvikt
Hjertesvikt, diagnostikk
Diagnosen mistenkes på grunnlag av de typiske symptomene. Det vil bli tatt blodprøver for å kartlegge sykdommen, og røntgenundersøkelse av brystet er også aktuelt for å skille hjertesykdom fra lungesykdom med lignende plager. EKG viser hos de fleste tegn til underliggende hjertesykdom. For bekreftelse av diagnosen er det nødvendig å foreta en ekkokardiografi, som er en ultralydundersøkelse av hjertet som foretas hos spesialist.
Hjertesvikt inndeles på bakgrunn av funn ved ekkokardiografi i 3 grupper, basert på "ejeksjonsfraksjon" (EF), d.v.s. hvor stor andel av hjertets hovedkammer som tømmes ved hvert hjerteslag. Inndelingen er (1) normal EF, (2) mildt redusert EF eller (3) redusert EF.
 AI-generert (ChatGPT 4o), prompt: Nicolas Øyane (NHI)
AI-generert (ChatGPT 4o), prompt: Nicolas Øyane (NHI)Hjertesvikt, behandling
Lettere grader av hjertesvikt behandles i allmennpraksis. Ved uttalt og akutt oppstått hjertesvikt er det nødvendig med sykehusbehandling i en periode. Hensikten med behandlingen er å lindre symptomene, bedre livskvaliteten og øke livslengden både via egenbehandling og medikamentell behandling.
Egenbehandling
Det er flere ting du selv kan gjøre:
- Spis mindre salt har lenge vært en anbefaling, fordi salt binder væske i kroppen og det kan øke belastningen på hjertet. Saltfattig kost synes å redusere symptomer, men det er ikke vist effekt på dødelighet eller sykehusinnleggelser. Det er derfor ikke grunn til å unngå alt salt. Myndighetene anbefaler maksimalt 5 gram salt daglig.
- Vær forsiktig med alkohol. Avholdenhet er sannsynligvis gunstigst, men unngå i alle fall mer enn 2-3 alkoholenheter om gangen, og unngå daglig bruk.
- Stump røyken.
- Det kan være nyttig å gå ned i vekt dersom du er overvektig.
- Fysisk aktivitet bør styres etter plagene. Klarer du regelmessig å mosjonere litt, er det nyttig. Men du bør ikke belaste mer enn det kroppen tillater.
Medikamentell behandling
Det finnes en rekke medikamenter som er effektive ved hjertesvikt. Det er spesielt ved gruppe (3) - redusert EF at medikamenter har stor betydning. Men også ved mildere grader av hjertesvikt kan noen medikamenter være aktuelle.
De viktigste medikamentgruppene er:
- ACE-hemmere og angiotensin II-antagonister (ARB) virker ved å utvide blodårene slik at blodtrykket går ned og belastningen på hjertet reduseres - de har ganske likeverdig effekt, og brukes ikke sammen.
- Kombinasjonspreparat med neprilysinhemmer og ARB utvider blodårer og medfører økt vannlatning, og har en gunstig effekt ved hjertesvikt med redusert EF. Denne medikamentgruppen erstatter eventuelt ACE-hemmer eller ARB dersom blodtrykket ikke er for lavt.
- Betablokkere får hjertet til å slå roligere, de senker blodtrykket og de styrker hjertet. Betablokkere brukes i tillegg til ett av de ovennevnte.
- SGLT-2-hemmere ble opprinnelig brukt for å senke blodsukker hos pasienter med diabetes, men har vist seg å bedre leveutsiktene hos pasienter ved alle grader av hjertesvikt, også til de som ikke har diabetes.
- Aldosteron-antagonister anbefales også til alle med hjertesvikt med redusert ejeksjonsfraksjon. Medikament-gruppen er mildt vanndrivende, og øker utskillelsen av kalium fra blodet, og har en gunstig effekt ved hjertesvikt
- Rene vanndrivende medisiner inngår ofte som tillegg til ovennevnte behandling, ev. ved behov med mye hevelse i kroppen.
- Digitalispreparater ble mye brukt før, men brukes sjelden nå
Oppsummert: Hos pasienter med hjertesvikt med redusert EF anbefales 4 ulike preparater samtidig: ACE-hemmer/ARB/ARB+neprilysinhemmer, betablokker, SGLT2-hemmer og aldosteron-antagonist. SGLT2-hemmer anbefales også ved mildt redusert og ved bevart EF. Valg av preparater og dosering styres av spesialist i hjertesykdommer, ev. i samarbeid med fastlege når tilstanden er stabil.
Blodfortynnende medisiner anbefales dersom du også har atrieflimmer. Dersom det er hjerteinfarkt eller angina som er årsak til hjertesvikten, vil de fleste anbefales behandling med såkalte statiner, det vil si medisiner som senker kolesterol.
Annen behandling
Årlig influensavaksine anbefales fordi det gir økt overlevelse hos pasienter med hjertesvikt. I tillegg anbefales også pneumokokk-vaksine hvert sjette år til alle som er over 65 år, og covid-vaksinasjon etter nasjonale faglige råd.
Hos noen kan det være aktuelt med kirurgi. Det gjelder særlig dersom det foreligger klaffefeil som kan repareres. Blant pasienter med tendens til alvorlige rytmeforstyrrelser kan det være aktuelt å operere inn en pacemaker eller en hjertestarter (ICD), eller kombinasjoner av dette. I svært sjeldne tilfeller gjøres hjertetransplantasjon.
Oppfølging ved hjertesvikt
Det kan lett bli mange ulike medisiner, spesielt hos eldre eller hos dem som også behandles for andre sykdommer. Det er en viktig del av legens oppfølging å kontrollere at ulike medisiner passer sammen, og at bivirkningene ikke blir større enn behandlingseffekten. Ha derfor alltid en nøyaktig medisinliste med til alle kontroller både på sykehus og til fastlege.
Pasienter med hjertesvikt følges ofte opp ved spesialiserte hjertesviktpoliklinikker. I starten er det hyppige kontroller i forbindelse med opptrapping av medisiner, deretter anbefales minst halvårlige kontroller. Disse vil av og til være hos hjertespesialist, av og til hos fastlege.
Daglige veiinger i starten kan bidra til å oppdage væskeopphopning (som følge av hjertesvikt) tidlig. Merk at en del medikamenter må pauses ved sykdom ved dehydrering, derfor er det viktig å kontakte lege ved sykdom.
Flere medisiner anbefales ikke brukt ved hjertesvikt, dette gjelder blant annet NSAIDs (ibuprofen, naproxen mm). Ta kontakt med lege eller farmasøyt for du starter på reseptfrie medikamenter.
Hjertesvikt, prognose
Kronisk hjertesvikt er en alvorlig tilstand der det allerede har oppstått varige forandringer i hjertet. Medikamentene som benyttes er til stor hjelp og bidrar i betydelig grad til å lindre plager og forlenge livet.
Hvor god prognosen er, vil avhenge av hvor alvorlig hjertesvikten er.
Når bør du kontakte lege?
Ved akutte alvorlige symptomer, kontakt legevakt (telefon 116117) eller ring 113.
Dette gjelder dersom du har:
- Alvorlig tung pust, pustevansker eller kvelningsfornemmelse
- Plutselig sterke brystsmerter
- Besvimelse eller alvorlig svimmelhet
Ta kontakt med fastlegen din hvis du opplever symptomer som kan tyde på hjertesvikt:
- Vedvarende tung pust, spesielt i hvile eller når du legger deg ned
- Hovne ankler, bein eller mage (væskeansamling)
- Uforklarlig slapphet, økt trettbarhet eller nedsatt yteevne
- Uvanlig hjertebank, svimmelhet eller besvimelsesanfall
- Redusert matlyst eller uforklarlig vektøkning
Merk at disse plagene kan ha mange årsaker, men det er viktig at en lege vurderer deg, spesielt hvis du har risikofaktorer som høyt blodtrykk, gjennomgått hjerteinfarkt, diabetes eller annen hjertesykdom.
Dersom du allerede er under behandling for hjertesvikt
Kontakt lege dersom du opplever:
- Rask vektøkning (mer enn 2 kg på 1–3 dager)
- Forverring av tung pust, spesielt i hvile eller om natten
- Hovne bein eller mage som blir tydelig verre
- Plutselig økt tretthet, svimmelhet, hjertebank eller besvimelsesanfall
- Uvanlig tørrhoste, surkling i brystet eller nattlig hoste
- Redusert urinmengde, eller tegn til uttørking (spesielt ved feber, oppkast eller diaré)
- Sterk hjertebank eller uregelmessig puls
Vær også oppmerksom dersom du får bivirkninger av medisiner, eller er usikker på egen behandling. God oppfølging og tidlig kontakt med lege kan bidra til å forhindre forverring av hjertesvikt.
Dette dokumentet er basert på det profesjonelle dokumentet Hjertesvikt, kronisk . Referanselisten for dette dokumentet vises nedenfor
- McDonagh TA, Metra M, Adamo M, et al. 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: Developed by the Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC) With the special contribution of the Heart Failure Association (HFA) of the ESC. Eur Heart J 2021. doi:10.1093/eurheartj/ehab368 DOI
- Criteria Committee of the New York Heart Association. Nomenclature and criteria for diagnosis of diseases of the heart and great vessels. 9th ed. Boston: Little, Brown, 1994.
- Kringeland, E., Slungård, G. F., Forster, R. B., Akerkar, R., & Eriksen, S. H. W. (2023). Hjerte- og karregisteret – Rapport for 2022. Folkehelseinstituttet. www.fhi.no
- Folkehelseinstituttet. Forekomst av hjerte- og karsykdommer i 2020. FHI 2021. www.fhi.no
- Gullestad L og Broch K. Kronisk hjertesvikt anno 2022. Hjerteforum 2022; 35: 14-26. www.legeforeningen.no
- Chioncel O, Lainscak M, Seferovic PM, et al. Epidemiology and one-year outcomes in patients with chronic heart failure and preserved, mid-range and reduced ejection fraction: an analysis of the ESC Heart Failure Long-Term Registry. Eur J Heart Fail. 2017 Dec;19(12):1574-1585. Epub 2017 Apr 6. PMID: 28386917.
- Aarønæs M, Atar D, Bonarjee V, et al. Kronisk hjertesvikt - etiologi og diagnostikk. Tidsskr Nor Lægeforen 2007; 127: 171-3. PubMed
- Rush CJ, Berry C, Oldroyd KG, et al. Prevalence of Coronary Artery Disease and Coronary Microvascular Dysfunction in Patients With Heart Failure With Preserved Ejection Fraction. JAMA Cardiol 2021. pmid:34160566 PubMed
- Abraham WT, Fisher WG, Smith AL, et al. Cardiac resynchronization in chronic heart failure. N Engl J Med 2002; 346: 1845-53. PubMed
- Neilan TG, Quinaglia T, Onoue T, et al. Atorvastatin for Anthracycline-Associated Cardiac Dysfunction The STOP-CA Randomized Clinical Trial. JAMA 2023; 330: 528-536. pmid:37552303 PubMed
- Utredning, behandling og oppfølging av hjertesvikt i allmennpraksis. Veileder utarbeidet av arbeidsgruppen for hjertesvikt i Norsk cardiologisk selskap. Versjon august 2024. Lest 14.10.2024 www.legeforeningen.no
- Fuery MA, Leifer ES, Samsky MD, et al. Prognostic Impact of Repeated NT-proBNP Measurements in Patients With Heart Failure With Reduced Ejection Fraction. JACC Heart Fail 2023. pmid:38127049 PubMed
- Dosh SA. Diagnosis of heart failure in adults. Am Fam Physician 2004; 70: 2145-52. PubMed
- Real J, Cowles E, Wierzbicki AS, et al. Chronic heart failure in adults: summary of updated NICE guidance. BMJ 2018; 362: k3646. PMID: 30249604 PubMed
- Modin D, Jørgensen ME, Gislason G, et al. Influenza Vaccine in Heart Failure: Cumulative Number of Vaccinations, Frequency, Timing, and Survival: A Danish Nationwide Cohort Study. Circulation 2018. pmid:30586760 PubMed
- Folkehelseinstituttet. Pneumokokkvaksine - veileder for helsepersonell. Sist oppdatert 27.09.2022. Siden lest 18.10.2022 www.fhi.no
- Zhao Q, Chen C, Zhang J, et al. Effects of self-management interventions on heart failure: Systematic review and meta-analysis of randomized controlled trials. Int J Nurs Stud. 2020 Jun 16;110:103689. PMID: 32679402 PubMed
- Colin-Ramirez E, Sepehrvand N, Rathwell S, Ross H, Escobedo J, Macdonald P, Troughton R, Saldarriaga C, Lanas F, Doughty R, McAlister FA, Ezekowitz JA. Sodium Restriction in Patients With Heart Failure: A Systematic Review and Meta-Analysis of Randomized Clinical Trials. Circ Heart Fail. 2023 Jan;16(1):e009879. PMID: 36373551 PubMed
- Ezekowitz JA, Colin-Ramirez E, Ross H, et al. Reduction of dietary sodium to less than 100 mmol in heart failure (SODIUM-HF): an international, open-label, randomised, controlled trial. Lancet 2022; 399: 1391-1400. pmid:35381194 PubMed
- Mandras SA, Uber PA, Mehra MR. Sexual activity and chronic heart failure. Mayo Clin Proc 2007; 82: 1203-10. PubMed
- Rizos EC, Ntzani EE, Bika E, et al. Association between omega-3 fatty acid supplementation and risk of major cardiovascular disease. JAMA 2012; 308: 1024-33. Journal of the American Medical Association
- Suebsaicharoen T, Chunekamrai P, Yingchoncharoen T, et al. Comparative cardiovascular outcomes of novel drugs as an addition to conventional triple therapy for heart failure with reduced ejection fraction (HFrEF): a network meta-analysis of randomised controlled trials. OpenHeart 2023; 10: e002364. pmid:37940331 PubMed
- Anker SD, Butler J, Filippatos G, et al. Empagliflozin in Heart Failure with a Preserved Ejection Fraction. N Engl J Med 2021. pmid:34449189 PubMed
- Vaduganathan M, Docherty KF, Claggett BL, et al. SGLT-2 inhibitors in patients with heart failure: a comprehensive meta-analysis of five randomised controlled trials. Lancet 2022. doi:10.1016/S0140-6736(22)01429-5 DOI
- Solomon SD, McMurray JJV, Claggett B, et al. Dapagliflozin in Heart Failure with Mildly Reduced or Preserved Ejection Fraction. N Engl J Med 2022. doi:10.1056/NEJMoa2206286 DOI
- Mc Causland FR, Claggett BL, Vaduganathan M, et al. Dapagliflozin and Kidney Outcomes in Patients With Heart Failure With Mildly Reduced or Preserved Ejection Fraction A Prespecified Analysis of the DELIVER Randomized Clinical Trial. JAMA Cardiol 2022. pmid:36326604 PubMed
- Butler J, Usman MS, Filippatos G, et al. Safety and Efficacy of Empagliflozin and Diuretic Use in Patients with Heart Failure and Preserved Ejection Fraction A Post Hoc Analysis of the EMPEROR-Preserved Trial. JAMA Cardiol 2023. pmid:37223933 PubMed
- Butler J, Filippatos G, Siddiqi TJ, et al. Empagliflozin, health status, and quality of life in patients with heart failure and preserved ejection fraction: The EMPEROR-Preserved Trial. Circulation 2021. pmid:34779658 PubMed
- Kosiborod MN, Bhatt AS, Claggett BL, et al. Effect of Dapagliflozin on Health Status in Patients With Preserved or Mildly Reduced Ejection Fraction. J Am Coll Cardiol. 2022. PMID: 36526515 PubMed
- McDonagh TA, Metra M, Adamo M, et al. 2023 Focused Update of the 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: Developed by the task force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC) With the special contribution of the Heart Failure Association (HFA) of the ESC. Eur Heart J 2023. doi:10.1093/eurheartj/ehad195 DOI
- Kosiborod MN, Verma S, Borlaug BA, et al. Effects of Semaglutide on Symptoms, Function, and Quality of Life in Patients with Heart Failure with Preserved Ejection Fraction and Obesity: A Prespecified Analysis of the STEP-HFpEF Trial. Circulation 2023. PMID: 37952180 PubMed
- Butler J, Shah SJ, Petrie MC, et al. Semaglutide versus placebo in people with obesity-related heart failure with preserved ejection fraction: a pooled analysis of the STEP-HFpEF and STEP-HFpEF DM randomised trials. Lancet 2024; 403: 1635-1648. pmid:38599221 PubMed
- Petrie MC, Verma S, Docherty KF, et al. Effect of Dapagliflozin on Worsening Heart Failure and Cardiovascular Death in Patients With Heart Failure With and Without Diabetes. JAMA 2020; 323: 1353-68. pmid:32219386 PubMed
- Writing Committee; Maddox TM, Januzzi JL, Allen LA, et al. 2021 Update to the 2017 ACC Expert Consensus Decision Pathway for Optimization of Heart Failure Treatment: Answers to 10 Pivotal Issues About Heart Failure With Reduced Ejection Fraction: A Report of the American College of Cardiology Solution Set Oversight Committee. J Am Coll Cardiol 2021; 77: 772-810. pmid:33446410 PubMed
- Svanström H, Mkoma GF, Hviid A, Pasternak B. SGLT-2 inhibitors and mortality among patients with heart failure with reduced ejection fraction: linked database study. BMJ 2024; 387: e800925. pmid:39505389 PubMed
- Zou X, Shi Q, Vandvik PO, et al. Sodium-Glucose Cotransporter-2 Inhibitors in Patients With Heart Failure : A Systematic Review and Meta-analysis. Ann Intern Med. 2022. PMID: 35404670 PubMed
- Berg DD, Jhund PS, Docherty KF, et al. Time to Clinical Benefit of Dapagliflozin and Significance of Prior Heart Failure Hospitalization in Patients With Heart Failure With Reduced Ejection Fraction. JAMA Cardiol 2021; 6: 499-507. pmid:33595593 PubMed
- Docherty KF, Jhund PS, Claggett B, et al. Extrapolating Long-term Event-Free and Overall Survival With Dapagliflozin in Patients With Heart Failure and Reduced Ejection Fraction An Exploratory Analysis of a Phase 3 Randomized Clinical Trial. JAMA Cardiol 2021. doi:10.1001/jamacardio.2021.2632 DOI
- Biegus J, Voors AA, Collins SP, et al. Impact of empagliflozin on decongestion in acute heart failure: the EMPULSE trial. Eur Heart J. 2022. PMID: 36254693 PubMed
- Ferreira JP, Zannad F, Butler J, et al. Empagliflozin and serum potassium in heart failure: an analysis from EMPEROR-Pooled. Eur Heart J 2022. pmid:35687107 PubMed
- Joshi SJ, Singh T, Newby DE, Singh J. Sodium-glucose co-transporter 2 inhibitor therapy: mechanisms of action in heart failure. Heart 2021. pmid:33637556 PubMed
- Causland FRM, Claggett B, Vaduganathan M, et al. Decline in Estimated Glomerular Filtration Rate After Dapagliflozin in Heart Failure With Mildly Reduced or Preserved Ejection Fraction: A Prespecified Secondary Analysis of the DELIVER Randomized Clinical Trial. JAMA Cardiol 2023. pmid:37952176 PubMed
- Savage HO, Dimarco AD, Li B, et al. Sequencing of medical therapy in heart failure with a reduced ejection fraction. Heart 2022. pmid:36368882 PubMed
- MERIT-HF Study Group. Effect of metoprolol CR/XL in chronic heart failure: metoprolol CR/XL randomized intervention trial in congestive heart failure. Lancet 1999; 353: 2001-07.
- Pitt B, Pfeffer MA, Assmann SF, et al. Spironolactone for heart failure with preserved ejection fraction. N Engl J Med. 2014; 370:1383-92. doi: 10.1056/NEJMoa1313731 DOI
- Filippatos G, Anker SD, Agarval R, et al. Finerenone Reduces Risk of Incident Heart Failure in Patients With Chronic Kidney Disease and Type 2 Diabetes: Analyses from the FIGARO-DKD Trial. Circulation 2021. pmid:34775784 PubMed
- Oraii A, Healey JS, Kowalik K, et al. Mineralocorticoid receptor antagonists and atrial fibrillation: a meta-analysis of clinical trials. Eur Heart J 2024. pmid:38195054 PubMed
- Heidenreich PA, Bozkurt B, Aguilar D, et al. 2022 ACC/AHA/HFSA Guideline for the Management of Heart Failure: Executive Summary. J Card Fail 2022; 28: 810-830. pmid:35378259 PubMed
- Nielsen EE, Feinberg JB, Bu F-L, et al. Beneficial and harmful effects of sacubitril/valsartan in patients with heart failure: a systematic review of randomised clinical trials with meta-analysis and trial sequential analysis. Open Heart 2020; 7: e001294. pmid:33257469 PubMed
- Foa A, Vaduganathan M, Claggett BL, et al. Sacubitril/Valsartan-Related Hypotension in Patients With Heart Failure and Preserved or Mildly Reduced Ejection Fraction. J Am Coll Cardiol 2024; 83: 1731-1739. pmid:38537919 PubMed
- McMurray JJV, Jackson AM, Lam CSP, et al. Effects of sacubitril-valsartan, versus valsartan, in women compared to men with heart failure and preserved ejection fraction: Insights from PARAGON-HF. Circulation 2019. PMID: 31736337 PubMed
- Swedberg K, Komajda M, Böhm M, et al. Ivabradine and outcomes in chronic heart failure (SHIFT): a randomised placebo-controlled study. Lancet 2010; 376: 875-85. PMID: 20801500 PubMed
- Armstrong PW, Pieske B, Anstrom KJ, et. al, VICTORIA Study Group. Vericiguat in patients with heart failure and reduced ejection fraction. N Engl J Med 2020;382:1883–1893. PMID: 32222134 PubMed
- Liew AY, Eikelboom JW, Connolly SJ, et al. Efficacy and safety of warfarin vs. antiplatelet therapy in patients with systolic heart failure and sinus rhythm: a systematic review and meta-analysis of randomized controlled trials. Int J Stroke. 2014 ;9(2):199-206. doi: 10.1111/ijs.12036 DOI
- Lip GYH, Shantsila E. Anticoagulation versus placebo for heart failure in sinus rhythm. Cochrane Database of Systematic Reviews 2014, Issue 3. Art. No.: CD003336. DOI: 10.1002/14651858.CD003336.pub3. Accessed 13 April 2021 The Cochrane Library
- Wang TJ, Larson MG, Levy D et al. Temporal relations of atrial fibrillation and congestive heart failure and their joint influence on mortality: the Framingham Heart Study. Circulation 2003; 107: 2920-5. Circulation
- Pasqualotto E, Ternes CMP, Chavez MP, et al. Catheter ablation for atrial fibrillation in heart failure with reduced ejection fraction patients: A meta-analysis. Heart Rhythm 2024. pmid:38705438 PubMed
- Graham FJ, Guha K, Cleland JG, et al. Treating iron deficiency in patients with heart failure: what, why, when, how, where and who. Heart 2024. pmid:39160066 PubMed
- Ponikowski P, Kirwan B-A, Anker SD, et al on behalf of the AFFIRM-AHF Investigators. Ferric carboxymaltose for iron deficiency at discharge after acute heart failure: A multicentre, double-blind, randomised, controlled trial. Lancet 2020. PMID: 33197395 PubMed
- Kalra PR, Cleland JGF, Petrie MC, et al. Intravenous ferric derisomaltose in patients with heart failure and iron deficiency in the UK (IRONMAN): an investigator-initiated, prospective, randomised, open-label, blinded-endpoint trial. Lancet 2022; 400: 2199-2209. pmid:36347265 PubMed
- Mentz RJ, Garg J, Rockhold FW, et al. Ferric Carboxymaltose in Heart Failure with Iron Deficiency. N Engl J Med 2023. doi:10.1056/NEJMoa2304968 DOI
- McMurray JJV, Solomon SD, Inzucchi SE, et al. Dapagliflozin in Patients with Heart Failure and Reduced Ejection Fraction. N Engl J Med 2019. pmid:31535829 PubMed
- Zhou X, Xu W, Xu Y, et al. Iron Supplementation Improves Cardiovascular Outcomes in Patients with Heart Failure. Am J Med. 2019. PMID: 30853478 PubMed
- Schou M, Gustafsson F, Videbaek L, et al. Extended heart failure clinic follow-up in low-risk patients: a randomized clinical trial (NorthStar). Eur Heart J. 2012 Aug 8. pmid:PMID: 22875412 PubMed
- Long L, Mordi IR, Bridges C, et al. Exercise‐based cardiac rehabilitation for adults with heart failure. Cochrane Database of Systematic Reviews 2019, Issue 1. Art. No.: CD003331. DOI: 10.1002/14651858.CD003331.pub5. The Cochrane Library
- Pandey A, Parashar A, Kumbhani DJ, et al. Exercise training in patients with heart failure and preserved ejection fraction: meta-analysis of randomized control trials. Circ Heart Fail. 2015;8(1):33-40. doi: 10.1161/CIRCHEARTFAILURE.114.001615. DOI
- Mueller S, Winzer EB, Duvinage A, et al. Effect of High-Intensity Interval Training, Moderate Continuous Training, or Guideline-Based Physical Activity Advice on Peak Oxygen Consumption in Patients With Heart Failure With Preserved Ejection Fraction A Randomized Clinical Trial. JAMA 2021; 325: 542-51. pmid:33560320 PubMed
- Wang C, Xing J, Zhao B, Wang Y, Zhang L, Wang Y, Zheng M, Liu G. The Effects of High-Intensity Interval Training on Exercise Capacity and Prognosis in Heart Failure and Coronary Artery Disease: A Systematic Review and Meta-Analysis. Cardiovasc Ther. 2022 Jun 9;2022:4273809. MCID: PMC9203221
- Rangaswami J, Bhalla V, Blair JEA, Chang TI, Costa S, Lentine KL, Lerma EV, Mezue K, Molitch M, Mullens W, Ronco C, Tang WHW, McCullough PA; American Heart Association Council on the Kidney in Cardiovascular Disease and Council on Clinical Cardiology. Cardiorenal Syndrome: Classification, Pathophysiology, Diagnosis, and Treatment Strategies: A Scientific Statement From the American Heart Association. Circulation. 2019 Apr 16;139(16). PMID: 30852913. PubMed
- Ostrominski JW, Greene SJ, Patel RB, et al. Kidney Outcomes Among Medicare Beneficiaries After Hospitalization for Heart Failure. JAMA Cardiol 2024. pmid:38809567 PubMed
- Silverberg DS, Wexler D, Sheps D, Blum M, Keren G, Baruch R, Schwartz D, Yachnin T, Steinbruch S, Shapira I, Laniado S, Iaina A. The effect of correction of mild anemia in severe, resistant congestive heart failure using subcutaneous erythropoietin and intravenous iron: a randomized controlled study. J Am Coll Cardiol. 2001 Jun 1;37(7):1775-80. PMID: 11401110 PubMed
- Hsu JJ, Ziaeian B, Fonarow GC. Heart Failure With Mid-Range (Borderline) Ejection Fraction: Clinical Implications and Future Directions. JACC Heart Fail. 2017 Nov;5(11):763-771.Eub 2017 Oct 11. PMID: 29032140 PubMed
- Tsimploulis A, Lam PH, Arundel C, et al. Systolic blood pressure and outcomes in patients with heart failure with preserved ejection fraction. JAMA Cardiol 2018. pmid:29450487 PubMed
- Taylor CJ, Lay-Flurrie SL, Ordóñez-Mena JM, et al. Natriuretic peptide level at heart failure diagnosis and risk of hospitalisation and death in England 2004–2018. Heart 2021. pmid:34183432 PubMed
- Taylor CJ, Ordonez-Mena JM, Roalfe AK, et al. Trends in survival after a diagnosis of heart failure in the United Kingdom 2000-2017: population based cohort study. BMJ. 2019 Feb 13;364:l223. PMID: 30760447 PubMed
- Berge K, Brynildsen J, Røysland R, et al. Prognostic value of cardiac biomarkers and National Early Warning Score 2 in acute dyspnoea. Open Heart 2022. pmid:35387863 PubMed
- Norsk kvalitetsforbedring av laboratorieundersøkelser (Noklus). Anbefalte analyser ved ulike kliniske problemstillinger. Siden besøkt 21.09.2020. www.noklus.no